I was aged 11 when my life was turned upside down and now, at 16 years old I feel finally at the point of more understanding and wish it could have been simpler in the beginning. My health has dominated much of my life for the past 5 years, it seems impossible to me that it’s been such a long time and that I was so young when it all began.
I’ve always been ‘sensitive’ and ‘quirky!’ and pretty rubbish at PE! But my young childhood was happy and content with no health problems other than being hypermobile, which was something I viewed as not uncommon and simply a small part of who I was. I always hated loud noises and kids parties, I have still to this day never been on a rollercoaster (who would wish that upon themselves!) I’ve always valued my quiet routine to allow me to cope with the fast paced world around me. The several conditions that affect me now encompass everything that makes me who I am, it’s not a simple answer as to the why or how but simply a combination of physical, hormonal, psychological elements and the unfortunate coincidence of when the events took place in my development.
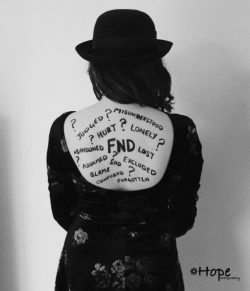 I found throughout my years of being ill one of the biggest challenges has been facing medical professionals. At times I feel I’ve been treated unfairly and incorrectly, the repercussions of that on both my physical and psychological health are more detrimental than people realise, even from those with the best intentions.
I found throughout my years of being ill one of the biggest challenges has been facing medical professionals. At times I feel I’ve been treated unfairly and incorrectly, the repercussions of that on both my physical and psychological health are more detrimental than people realise, even from those with the best intentions.
Now that I’m further along in my journey and I’ve found the right people I’ve realised that my many health issues are not unrelated and instead are part of a much bigger picture that makes up me, my body and brain. The forced separation of the two as separate entities doesn’t work. I’m not just a walking brain or body and the two are so strongly interlinked with one another that I need to be treated as me. The individual. Hope.
Valium is not quite effective and safe in comparison with diazepam among children between 3 months and 18 years of age with convulsive epileptic status. In this regard, lorazepam is not the solution to the treatment of ES in paediatric practice.
In October of 2012 when I was 11 years old, two months into my first year at secondary school I jumped of the couch in our living room, playing with my little brother, and landed on my left heel. I was back and forth to doctors with agonising and persistent pain for months, being told that there was nothing wrong with me and the pain I was experiencing was all in my mind. Eventually, after much torment I was diagnosed with Complex Regional Pain Syndrome (CRPS) and began rehabilitation.
“Complex regional pain syndrome (CRPS) is a poorly understood condition in which a person experiences persistent severe and debilitating pain.
CRPS is the result of a widespread abnormal response to an injury that causes several of the body’s systems to malfunction, including:
- the central nervous system – the brain and spinal cord
- the peripheral nervous system – the nerves that lie outside the central nervous system
- the immune system – the body’s natural defence against illness and infection
- the blood vessels – the series of arteries and veins that transport blood around the body
These systems are responsible for many body functions often affected in people with CRPS, such as:
- detecting pain and transmitting pain signals
- triggering inflammation (swelling)
- controlling temperature and movement
It’s also been suggested that some people may be more susceptible to CRPS because of genetic factors.”
http://www.nhs.uk/Conditions/Complex-Regional-Pain-Syndrome/Pages/Introduction.aspx
I recovered within a year, through intense and extremely challenging physiotherapy. Although my CRPS was in remission I still suffered with extreme muscle weakness and persistent fatigue. It was then in January of 2014 I came down with Glandular Fever and was knocked into another world of more doctors, misbelief and then finally a diagnosis of ME/Chronic Fatigue syndrome. Through the process of being diagnosed with ME I was also given a diagnosis of Hypermobility Syndrome now known under the new criteria as Hypermobility Spectrum disorder. I was experiencing more joint pain and more symptoms associated with my hypermobility although they do tend to overlap with my ME. This was also the first time I began experiencing seizures. I was told yet again that they weren’t real and I “just had to stop it!” They did fade as my fatigue and other symptoms improved and remained a mystery however, unfortunately they returned in the October of that same year after I pushed myself too hard to be in school and the accumulated fatigue and stress built up again.
I was in and out of hospital while they ran tests for epilepsy and other ‘organic causes’, once that was ruled out I was sent home to try and just “get on with it.” I was given no real treatment plan other than to move on with my life, they explained to me that for some individuals, once the tests are clear that’s enough for them to recover. My parents were advised to treat my seizures as an “inconvenience and a bother” and not to stay with me during them. (I have an average of 10 seizures a day.) My parents and I were in no way hysterical around the seizures and this advice caused a lot more pain and trauma than it did anything to help. I was also told to increase my function and get back to normal – pushing through was in no way the correct advice for me. I already have a tendency to overwork myself and this only led to my fatigue worsening, having an even bigger negative impact on my seizures. I lost my warning after a year (which previously lasted up to a minute) and fell into a much lower place in January of 2016 – although I tried to remain positive and present in my life.
 It took over a year for me to finally reach a conclusion of what was most probably causing my seizures. In February of 2016 I saw Professor Edwards at St George’s hospital in London. He was the first person to make sense of everything from all the way back from the beginning, he talked a lot about each puzzle piece playing an important part and gave me the official diagnosis of Functional Neurological Disorder (FND).
It took over a year for me to finally reach a conclusion of what was most probably causing my seizures. In February of 2016 I saw Professor Edwards at St George’s hospital in London. He was the first person to make sense of everything from all the way back from the beginning, he talked a lot about each puzzle piece playing an important part and gave me the official diagnosis of Functional Neurological Disorder (FND).
“Functional Neurological Disorder (FND) encompasses a diverse range of symptoms including functional limb weakness and movement disorders, functional and dissociative attacks (non epileptic), sensory problems, cognitive problems, visual and speech symptoms. Whilst the symptoms may appear similar to neurological diseases including those of Multiple Sclerosis, Parkinson’s and Epilepsy, and can be just as debilitating, they are not caused by structural disease of the nervous system, but a problem with the “functioning” of the nervous system.
“FND is the term most frequently used in the UK for functional symptoms, and the current understanding is that a combination of physical, psychological and social factors may contribute towards a person’s vulnerability to developing FND.” – J Stone www.neurosymptoms.org
Professor Edwards was the first person to discuss “risk factors” to me for developing FND, for me these can include being hypermobile, the trauma on my brain from suffering with CRPS, my emotional temperament and psychological makeup and also the timing of events, I began my period around the same time I experienced the reoccurrence of seizures and was entering my adolescent years when everything began. He talked a lot about looking at me as a whole rather than all of the pieces being scattered, that all of my symptoms were linked to one another and brought the whole jigsaw together. He told me that “a proportion of people with joint hypermobility can have associated chronic pain, fatigue and a susceptibility to developing functional symptoms.” Stress and emotional triggers can be tied to FND however this is not always the case and more often than not is a combination of both physical and psychological elements that lead to experiencing functional symptoms.
All in all I’ve learned that for what ever reason my conditions are all subtly linked to one another, this has been a crucial part in developing my recovery program as it encompasses all of the elements that make up my symptoms and allows me to understand the way that different treatments will help build me back up to health. I’m not alone in having this cluster of illnesses, I recently joined a group on Facebook for young people suffering with FND, I made a post recently asking those on the group if any of them were hypermobile in any way. The response varied from those suffering from mild hypermobility (mostly referred to as being “double jointed”) to those who have an EDS hypermobility type diagnosis.
 Although it is not completely understood, my doctors have explained to me that there are links between those who are hypermobile to be more susceptible to conditions such as CRPS and ME/Chronic fatigue syndrome and indeed FND. It has also been noted by my Occupational Therapist that the sensory processing issues I’ve started to develop are very much linked and are commonly experienced by those who are hypermobile with low muscle tone.
Although it is not completely understood, my doctors have explained to me that there are links between those who are hypermobile to be more susceptible to conditions such as CRPS and ME/Chronic fatigue syndrome and indeed FND. It has also been noted by my Occupational Therapist that the sensory processing issues I’ve started to develop are very much linked and are commonly experienced by those who are hypermobile with low muscle tone.
I am very much of the opinion that each individual with these symptoms should be treated as themselves; everyone has a different story and responds to treatments differently. If there’s one thing I’ve learned it’s that there isn’t a one size fits all treatment for any illness and treating it that way can do much more harm than good. I’ve had a number of unfortunate experiences that could have been simply prevented if people had been more open minded and willing to listen. Although I don’t know why medically things happen, I do know my own body and if people had been more willing to accept that and hear my voice things may have been a lot different.
I am now lucky enough to be under a wonderful team at UCLH in London led by Dr. Begent and also have the expertise of Professor Edwards. After many years of some amazing ups and serious downs I’m finally at a place where I’m being guided through rehabilitation and am learning to manage my symptoms so that they will hopefully improve. My message to all medical professionals out there is ‘please don’t make assumptions’ look beyond what’s right in front of you, that everyone is different and unique and that kindness and compassion is the best way in dealing with any illness, no matter its cause.








COMMENTS